Dr. Clark, Director of USC’s Online Master’s Degree in Orofacial Pain and Oral Medicine, teaches dental residents how to map, cold test, and anesthetic test Allodynia Zones to diagnose Chronic Trigeminal Neuralgia.
Allodynia Mapping
Neuropathic pain almost always produces increased sensitivity to light touch. When this touch causes pain, this is called mechano-sensitive allodynia, and it can and should be mapped. Allodynia Mapping is important above and beyond confirming you have a neuropathic pain problem is that in Step #5a and #5b, we discuss how cold and anesthetic testing is used. However, these tests are only done in cases where you have a proven focal mechano-sensitive allodynia map.
Mechno-sensitive allodynia mapping is typically done with a Q-tip and one-side is compared to the other to find the area of unusual sensitivity. This allodynia can be intra-oral or extra-oral.
Like what you’re learning? Test your clinical diagnosis skills with USC’s Virtual Patient Simulation. Review real-life patient histories, symptoms, and imaging, conduct a medical interview and clinical exam, make a diagnosis, and create a treatment plan for virtual patients experiencing Orofacial Pain conditions.
Gingival Cold Testing the Allodynia Zone
We know that cold applied to a tooth with an inflamed pulp is more sensitive and more likely to produce lingering pain than a non-inflamed tooth. This same cold test for pulp vitality can be used on gingival tissues with proven allodynia.
Essentially, if the nerve supplying the gingiva is sensitized and exhibits mechano-allodynia, then this test can be used for two purposes. First, to confirm that the nerve is hyperactive, and second to see if the treatment is reducing the hyperactivity over time. In the latter case, the duration of the post-stimulation pain will reduce as the nerve regains normal sensitivity.
Gingival Cold Test Protocol
- Cotton swab (5 mm in diameter)
- Sprayed with Gebauer Ethyl Chloride
- Site located in the area of mechanical allodynia
- Cotton swab held in location for 3 sec.
- Pain & cold sensations rated 10-cm VAS or 0-10 numerical scale
- 0 = “no sensation” and 10 = “freezing cold” OR
- 0 = “no pain” 10 = “worst possible pain”]
- Post removal duration of pain or cold is timed
Method to Detect Gingival Neural Sensitization
Zagury JG et al. tested 21 patients with Atypical Odontalgia (AO) and 18 controls using Extraoral Quantitative Sensory Testing (electrical and thermal pain thresholds) and intraoral mucosal cold tests for prolonged gingival cold allodynia.
The results showed electrical pain thresholds were higher in AO patients, changes were in same as pain dermatome only, and the duration of cold pain was significantly longer in AO bilaterally. The extended painful aftersensation following cold application in AO patients supports the involvement of central mechanisms.
Anesthetic Testing for Pain Reduction in the Allodynia Zone
When you have gingival allodynia with ongoing pain, a good test to conduct is the anesthetic challenge test. This test can and should be used along with the clinical neurosensory examination when a suspected trigeminal neuropathy is suspected.
Anesthetic Challenge Test
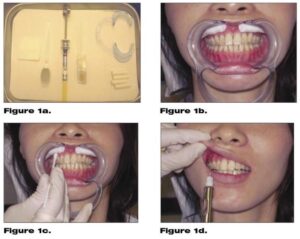
The Anesthetic Challenge Test involves isolating or mapping out the painful area, asking the patient to rate their ongoing spontaneous pain, and then applying either a topical anesthetic gel.
In cases where you are suspicious of the result, the test should be completed with a non-anesthetic gel (Vasoline(R)) to make sure the result is true, and this is best done on two separate days with the order of the test agents being applied randomly. Otherwise, anesthetic testing can be done in a single, blind fashion with a 30-minute washout period between agents, but the placebo agent must be used first. In either case, the patient will rate the pain change (if any) using the VAS scale.
The effect of topically applied benzocaine on spontaneous toothache without obvious cause was examined in 60 patients. Specifically, this study used a randomized, double-blind, placebo-controlled clinical trial to see the efficacy of intraoral benzocaine delivered via a patch at suppressing pain in spontaneous toothache pain of at least a moderate intensity.
They applied 12 mg of benzocaine or matching placebo on a patch approximately two millimeters apical to the mucogingival junction of the symptomatic tooth and remained in place for 60 minutes.
Using a survival analysis, they found that the percentage of patients reporting meaningful pain relief by 30 minutes was significantly (p < 0.05) greater in the benzocaine group than in the placebo group (77% for benzocaine and 47% for placebo).
Complete resolution of the chronic, otherwise unexplained trigeminal pain, with a topically applied anesthetic, indicates neuropathic pain with peripheral sensitization. Of course, this conclusion assumes all other local pathologies are not present, and a strong placebo effect is not present. In such cases, a custom fabricated vacuum formed tissue stent that covers the painful area can be made to hold the topical benzocaine in place for extended periods (Colgate Orabase-B®). The purpose of the stent is to hold the medication at the painful site. 1, 2, 3, 4
In the anesthetic test protocol, if the pain does not resolve with topical anesthetic, this lowers the chances of the sustained application being therapeutic and reversing the neuropathic changes. In these cases, the next step is to perform a local infiltration of the 2% lidocaine with epinephrine in the area to see if the pain can be stopped.
The neural changes are considered more substantial, and it is more likely that central sensitization has developed (i.e., 2nd and 3rd order neuronal changes) when a single anesthetic infiltration or nerve block fails. This suggests that the magnitude of peripheral and central change is such that the patients will require systemic (usually anticonvulsant) medications in addition to the topical anesthetics to manage the chronic pain.
Topical Anaesthesia & Persistent Dentoalveolar Pain (PDAP) Disorders
In this study, 25 subjects (19F:6M) with Persistent Dentoalveolar Pain (PDAP) were evaluated with a Quantitative Sensory Testing (QST) at a baseline and after a topical Benzocaine 2% against control of 25 health subject.
Results
- PDAP patients have lower pain detection thresholds (mechanical)
- PDAP patients have pain intensity reports (heat and cold)
- Topical Benzocaine reduces in 60% pain intensity in PDAP patients
In conclusion, PDAP patients had abnormal thermal, sensory, and mechanical allodynia. Topical anesthetics reduced pain detection with both mechanical and thermal testing.
Online Dental Specialty Training
Do you want to master a dental specialty while maintaining your dental practice? Consider enrolling in USC’s competency-based Master of Orofacial Pain and Oral Medicine degree program.
References:
- Merrill RL. Central mechanisms of orofacial pain. Dent Clin North Am. 2007 Jan;51(1):45-59.
- Svensson P, Petersen JK. Anesthetic effect of EMLA occluded with Orahesive oral bandages on oral mucosa. A placebo-controlled study. Anesth Prog. 1992;39(3):79-82.
- Svensson P, Petersen JK, Svensson H. Efficacy of a topical anesthetic on pain and unpleasantness during scaling of gingival pockets. Anesth Prog. 1994;41(2):35-9.
- Gupta AK, Sibbald RG. Eutectic lidocaine/prilocaine 5% cream and patch may provide satisfactory analgesia for excisional biopsy or curettage with electrosurgery of cutaneous lesions. A randomized, controlled, parallel group study. J Am Acad Dermatol. 1996 Sep;35(3 Pt 1):419-23.

