When dentists need to test for Obstructive Sleep Apnea or hypersomnolence, sleep-related questionnaires can be of help. The following post explores some of the interview questions clinicians use in their assessment.
Best Dental Questionnaires for OSA
In addition to conducting a comprehensive dental exam, and a medical interview, some clinicians use short sleep-related questionnaires such as (1) Modified Berlin questionnaire for OSA risk; and (2) Epworth Sleepiness Scale (ESS) Questionnaire to detect hypersomnolence.
The Berlin Questionnaire has several versions. The one listed below is the modified form of this questionnaire so that the questions are all yes/no in format. It is a reasonable predictor of Obstructive Sleep Apnea risk, especially when combined with a patients BMI score.
Like what you’re learning? Put it to the test with USC’s Virtual Patient Simulation. Review real-life patient histories, symptoms, and imaging, conduct a medical interview, perform a clinical exam, make your diagnosis, and create a treatment plan for virtual patients experiencing Orofacial Pain conditions.
Modified Berlin Questionnaire
- Do you snore loudly?
- Do you snore 3-4 times/week or more?
- Are you moderately sleepy during your waketime 3-4 times/week or more?
- Are you still tired after sleeping 3-4 times/week or more?
- Do awaken with a gasp for breath at least 3-4 times/week or more?
- Has anyone ever observed you stop breathing during your sleep for a few seconds?
- If you do stop breathing during sleep, do you have these breathing pauses 3-4
times/wk or more? - Does your snoring bother other people?
- Have you ever fallen asleep while driving?
- Do you have high blood pressure?
- Has anyone in your immediate genetic family been diagnosed with sleep apnea or were exceptionally loud snorers?
- Please list their relationship(s) to you.
Additional reading: Snoring Disorders for Dentists
Scoring the Modified Berlin
- At-Risk Group = Yes on both questions 4 & 6
- Medium Risk Group = Yes on at least two of questions 7, 8 or 9
- High-Risk Group = One of above plus “Yes” on questions 10 and a BMI > 30.
Epworth Sleepiness Questionnaire

The Epworth Sleepiness Scale (ESS) is designed to indicate sleepiness and is somewhat correlated with sleep apnea. The ESS questionnaire asks “how likely are you to doze off or of fall asleep in the following situations, in contrast to feeling just tired?” This
refers to your typical levels of sleepiness in the last month.
Epworth Sleepiness Questions
Choose the most appropriate number for each situation where (0) would never doze; (1) slight chance of dozing; (2) moderate chance of dozing; (3) high chance of dozing.
Score 0-3 Chance of Dozing for Each Situation
- Sitting and reading
- Watching TV
- Sitting, inactive in public place (e.g. theater/meeting).
- As a passenger in a car for an hour without a break.
- Lying down to rest in P.M. when the situation permits.
- Sitting and talking to someone.
- Sitting quietly after lunch without alcohol.
- In a car, while stopped for a few minutes in the traffic.
Sum the scores and a total greater than 10 is considered abnormal.
Daytime Sleepiness Questionnaires
You can use questionnaires to measure daytime sleepiness, but if the patient can lose their driver’s license if they fail, they may not be honest. In his study on the ESS Scale correctly measuring sleepiness of sleep apnea, Chevrin RD et al. determined occasional inconsistency.
ESS vs. Multiple Sleep Latency (MSL) Test
A 1999 study examined the utility of the Epworth sleepiness scale as a possible substitute for a Multiple Sleep Latency (MSL) test, the gold standard for daytime sleepiness questionnaires. If these two tests have a high correlation, then it makes sense to substitute the simpler questionnaire for the more complex daytime polysomnographic study known as a latency test.
In this study, 237 patients took the ESS and MSL test. 60% of patients (141 of 237) had a self-rating of sleepiness score, Polysomnograph (PSG), and Apnea–Hypopnea Index (AHI).
After regression models were conducted on data, the researchers found:
- ESS had a significant association with self-rated problem sleepiness.
- ESS did not correlate significantly with MSL or AHI score
- Male gender had considerably more influence on the ES than did MSL or AHI
The authors concluded that subjectively derived Epworth Sleepiness Scale cannot be used as a surrogate for the objectively determined Multiple Sleep Latency test.
Predicting Obstructive Sleep Apnea
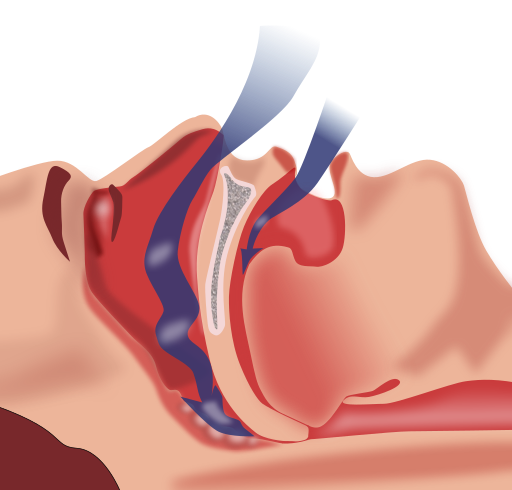
In 2010, Enciso R et al. studied the predictors of OSA using a combined imaging and questionnaire approach. Specifically, the gathered questionnaire data (using the Berlin Questionnaire OSA risk system) and supine airway CBCT images collected from polysomnography confirmed Obstructive Sleep Apnea and non-apnea snoring patients to develop a prediction model for OSA based on this data.
The study included 80 subjects (46 OSA patients with apnea-hypopnea index [AHI] greater than or equal to 10 and 34 snorers with an AHI less than 10 based on an ambulatory somnographic assessment. A multivariate logistic regression analysis was used to identify risk factors for OSA.
Additional reading: Imaging Obstructive Sleep Apnea & Sleep Disordered Breathing
The study reported:
- OSA patients were predominantly male and older and had a larger neck size and larger body mass index than the snorers;
- The minimum cross-sectional area of the upper airway and its lateral dimension were significantly smaller in the OSA patients;
- The minimum cross-sectional airway area divided by the average neck volume was significantly smaller in the OSA patients.
The logistic regression showed that OSA could be reliably predicted for patients who were > 57 years old, male gender, had a “high risk” score on the Berlin questionnaire, and narrow upper airway lateral dimension (<17 mm).
Predicting Hypertension
In 2008, a study by Gus M et al. examined the value of the Berlin Questionnaire as a predictor for hypertension. The authors speculated that since OSA is highly correlated with difficult to treat hypertension, a questionnaire which predicts OSA might also predict resistant hypertension.
The authors administered the Epworth Sleepiness Scale (ESS) and the Berlin Questionnaire to 63 patients with medication-resistant hypertension and 63 patients with medication controlled hypertension. The resistant hypertension cases all had a systolic (BP) > or =140 mm Hg or diastolic BP > or =90 mm Hg using at least three BP-lowering drugs, including a diuretic. All subjects in the study used an ambulatory BP monitoring device and a take-home polysomnographic device to gather their results.
The results showed that high OSA risk cases (defined via the Berlin Questionnaire) comprised 78% of the resistant hypertension group versus the 48% of the treated hypertension group (p < 0.001). The authors also found that a high-risk OSA score on the Berlin Questionnaire yielded an increased odds of resistant hypertension (odds ratio 4.1). Moreover, sensitivity and specificity for the diagnosis of OSA was 85.5% (75.3-92.0%) and 65.0% (52.0-76.0%) respectively.
Dental Masters Programs
Are you looking to expand care to patients suffering from Obstructive Sleep Apnea or other sleep breathing disorders, and maintain your practice? Check out USC’s online Orofacial Pain and Oral Medicine specialty training program.

