
The following equipment is required for a Cranial Nerve Examination:
- Cotton ball
- Safety pin
- Pen torch (source of light)
- Tongue blade
- Tuning fork (512 Hz)
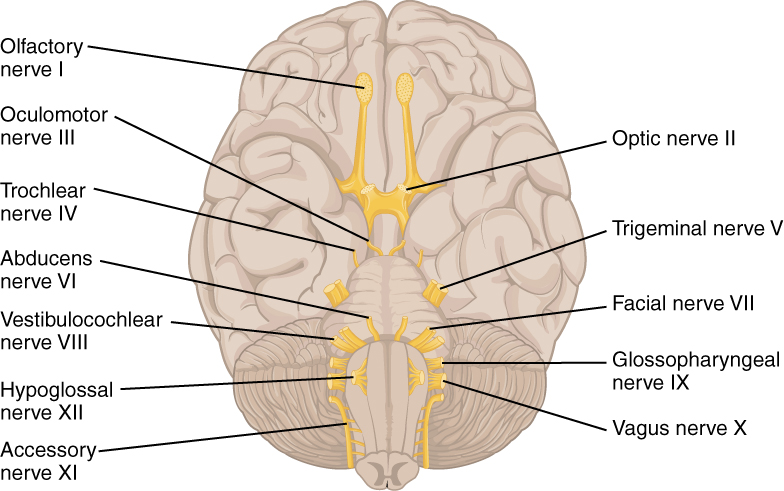
1.) Olfactory Nerve (I)
The olfactory is a sensory nerve, and damage in the nasal epithelium or the basal gangliamight impair the ability to discriminate different smells. The olfactory nerve can be tested using products with specific spices, so the patient can recognize the differences; however, usually just asking the patient: “Do you recognize different aromas?” is enough.
2.) Optic Nerve (II)
In this abbreviated exam we will test only reflex response for direct and concentric reflex to bright light. This is done by shining a pen torch into one eye and check that the pupils on both sides constrict. This should be tested on both sides. The common abnormalities include neuritis (related with loss of myelin), glaucoma and autoimmune conditions.
Like what you’re learning? Explore our online, postgraduate Orofacial Pain and Oral Medicine degrees.
3.) Oculomotor, Trochlear and Abducent Nerves (III, IV, VI)
These three nerves are tested together as the control movement of the eye. This is done by asking the patient to keep their head perfectly still directly in front of you, you should draw two large joining H’s in front of them using your finger and ask them to follow your finger with their eyes.
When the patient cannot track motion this means neurologic damage involving cranial nerves III, IV, or VI. The common abnormalities include brain tumor, hemorrhagic brain disease, stroke, and local eye disease damaging the muscles of ocular motion.
4.) Trigeminal Nerve (V) – Motor
To test the motor supply of patients, ask them to clench their teeth together while observing and feeling the bulk of the masseter and temporalis muscles. Then, ask the patient to open against resistance.
The eight muscles which the trigeminal motor nerve innervates are the masseter, temporalis, medial pterygoid, lateral pterygoid, mylohyoid, tensor tympani, tensor velialatine, and anterior belly of digastric.
The common abnormalities include disease of the muscle itself (myopathy), and motor nerve damage in peripheral/spinal cord/brain from cancer or trauma.
Note: Third division of trigeminal nerve innervates masseter and temporalis, so you should check for contraction of both muscles!
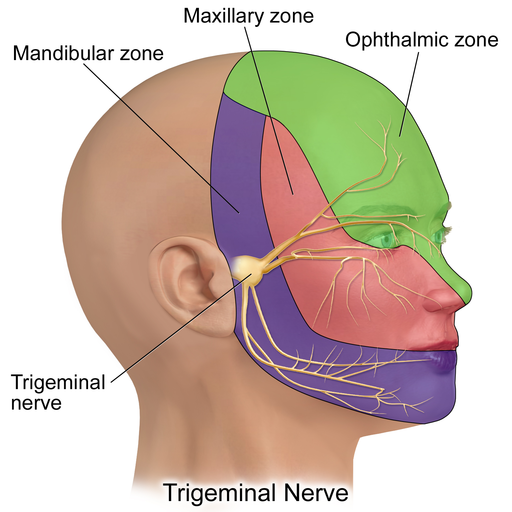
5.) Trigeminal Nerve (V) – Sensory
The trigeminal nerve provides sensory supply to the face and mouth. It has three sensory branches (ophthalmic, maxillary and mandibular), and it is tested by lightly touching the face with a piece of cotton wool followed by a blunt pin in each division on each side of the face.
Dermatome of V1, V2 & V3
The sensory nerve distributions of the trigeminal nerve on the face which are:
- Ophthalmic division: the forehead, upper eyelid, cornea, conjunctiva, and dorsum of the nose
- Maxillary division: the upper lip, lateral portions of nose, upper cheek, anterior temple, mucosa of nose, upper jaw, upper teeth, and roof of mouth
- Mandibular division: the lower lip, chin, posterior cheek, temple, external ear, mucosa of lower part of mouth, anterior two-thirds of the tongue, and it does not include the angle of mandible!
The common abnormalities include peripheral lesions (fracture, trauma, tumors, infections), lesions of the ganglion (Herpes zoster infection, primary/metastatic tumors), and trigeminal root lesions (adjacent tumors, vascular malformations).
Corneal Reflex
The corneal reflex should also be examined as the sensory supply to the cornea is from this nerve. Do this by lightly touching the cornea with the cotton wool, which causes the patient to shut both eyelids.
The corneal reflex has two parts: the sensory, or afferent, part of the reflex is mediated by the ophthalmic branch of the trigeminal nerve, and the motor, or efferent, part of the reflex is mediated by the facial nerve.
Like what you’re learning? Explore our online, postgraduate Orofacial Pain and Oral Medicine degrees.
(6) Facial Motor Nerve (VII)
The facial motor nerve supplies motor branches to the muscles of facial expression. This nerve is therefore tested by asking the patient to crease up their forehead by raising their eyebrows, close their eyes, and keep them closed against resistance, puff out their cheeks and reveal their teeth.
Facial Muscles
When the patient can raise their forehead bilaterally, but unilaterally the facial muscles are paralyzed, the problem is located in the upper motor neuron. When the patient has paralysis of one entire side (forehead, eyes, and perioral/smile) the problem is located in the lower motor neuron. The common abnormalities include Bell’s palsy, and motor nerve damage (neoplasm, trauma, middle ear infections, parotid gland surgery, granulomatous or carcinomatous meningitis, diabetes).
Taste
Taste buds on the anterior two thirds of the dorsal region of the tongue is innervated by CN VII. Sensory fibers of CN VII travel together with motor fibers of this nerve, but in the middle ear region, sensory fibers branch off to form the chorda tympani which then joins CN V lingual branch where it eventually enters the tongue. The posterior third of the tongue is supplied from CN IX that also provides parasympathetic fibers to the salivary glands but not taste.
7.) Vestibulocochlear Nerve (VIII)
The vestibulocochlear nerve provides innervation to the hearing apparatus of the ear and can be used to differentiate conductive and sensori-neural hearing loss using the Rinne and Weber tests.
Weber Test
Place the tuning fork base down in the center of the patient’s forehead and ask if it is louder in either ear. Normally it should be heard equally in both ears. If hearing is diminished as indicated on the finger rub, Weber test conduct the Rinne test.
Rinne Test
Place a tuning fork on the mastoid process and then next to their ear and ask which is louder (normally the second is louder).
8.) Glossopharyngeal Nerve (IX)
The glossopharyngeal nerve provides sensory supply to the palate. It can be tested with the gag reflex by touching the pharynx with a tongue depressor or by touching the arches of the pharynx.
9.) Vagus Nerve (X)
The vagus nerve provides motor supply to the pharynx. To test the vagus nerve, ask the patient to say “AH,” which will cause the pharynx to elevate, and observe the position of the uvula. When the palatal muscles works properly, the “AH,” sound should be clear and the uvula should not move to one side.
10.) Accessory Nerve (XI)
The accessory nerve gives motor supply to the sternocleidomastoid and trapezius muscles. Ask the patient to shrug their shoulders and turn their head against resistance. The common abnormalities include lower motor neuron (LMN) lesions which produce weakness of both muscles on the same side, upper motor neuron (UMN) lesions which produce ipsilateral sternocleidomastoid weakness and contralateral trapezius weakness, because of differing sources of cerebral innervation.
11.) Hypoglossal Nerve (XII)
The hypoglossal nerve provides motor supply to the muscles of the tongue. Check for fasciculation at rest, and ask the patient to to stick their tongue out. If the tongue deviates to either side, it suggests a weakening of the muscles on that side.
When the tongue deviates on protrusion, this suggests peripheral nerve damage on the side where the tongue is deviated. The common abnormalities include peripheral lesions that affect the nerve, brain metastases, and motor nerve damage from cancer or trauma.
Note: Once the examination is concluded, dispose the sharps and gloves accordingly with the standard biosecurity measurements, and explain to the patient any inconsistent or irregular finding and refer if appropriate.
Postgraduate Orofacial Pain and Oral Medicine Master’s Degree
Learn more about diagnosing, treating, and managing TMJ by enrolling in Herman Ostrow School of USC’s online, competency-based certificate or master’s program in Orofacial Pain and Oral Medicine.
