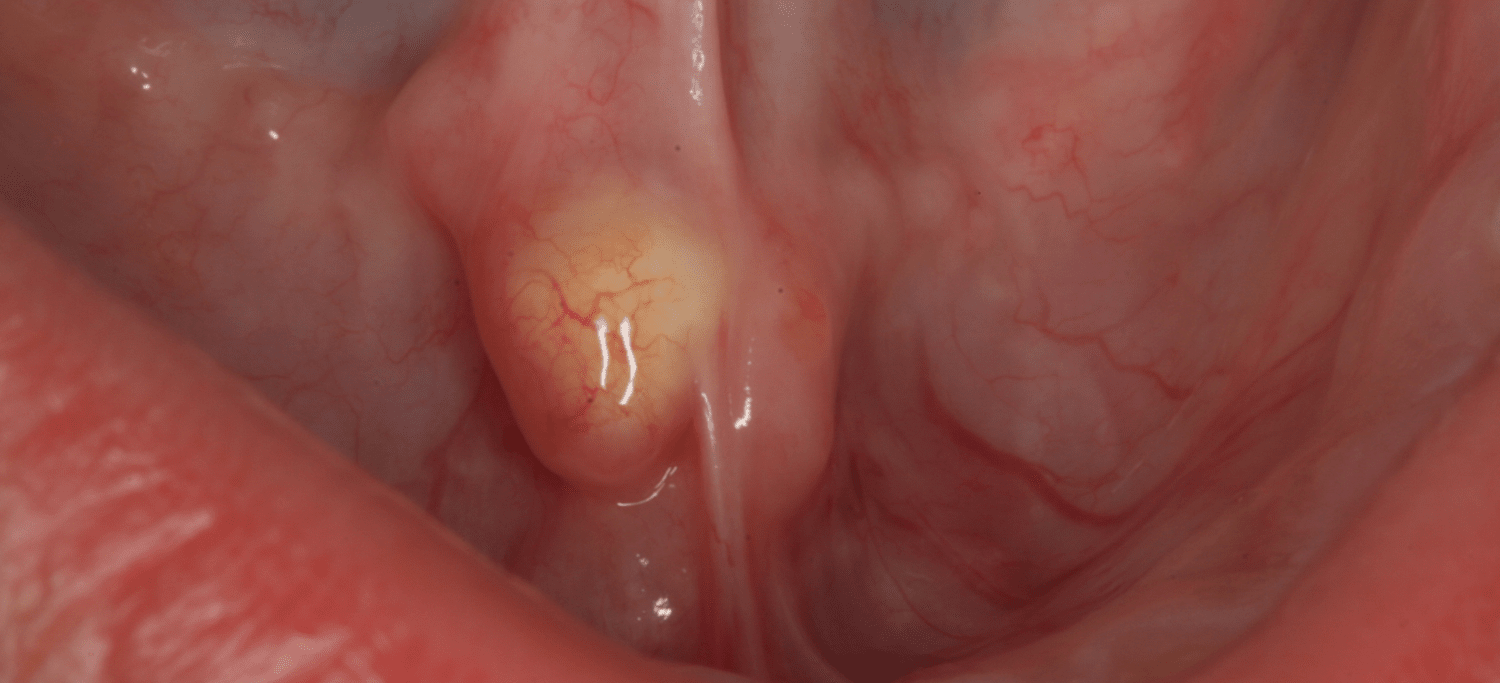
Figure. 1 – Sialolith in the right submandibular duct. Image courtesy of Dr. Al-Eryani, Orofacial Pain and Oral Medicine Center, Herman Ostrow School of Dentistry of USC)
What are salivary stones?
Salivary stones, also called sialoliths, are calcified organic masses that form within the salivary gland’s secretory system. Salivary stones comprise of organic and inorganic materials, including calcium carbonates and phosphates, cellular debris, glycoproteins, and mucopolysaccharides [1].
Related Reading: How to Perform a Salivary Gland and Salivary Flow Exam
Salivary Stone Formation Stages
- Decreased saliva flow
- Deposits settle in walls of salivary duct
- Flow of saliva slowed
- Deposits of calcium, phosphorus
- Forms small concretions (micro-stone)
- Grow into stone
- Stones block the duct
- Bacteria moves from the mouth up, around the blockage, into salivary duct
- Inflammation, tissue swelling (sialadenitis secondary to stone)
Related Reading: Understanding the Role of Saliva
Like what you’re learning? Download a brochure for our online, postgraduate Orofacial Pain and Oral Medicine degree program.
Etiological Factors for Salivary Stone Formation
The following are some of the etiological factors for salivary stone formation [2]:
- Abnormal narrowing of the salivary gland duct
- Salivary gland inflammation or infections
- Dehydration medications (i.e., antidepressants, anticholinergics, antispasmodics, antihistamines, antihypertensives)
- Saliva composition (i.e., calcium saturation)
- A deficit of crystallization inhibitors (i.e., phytate)
Related Reading: Diseases and Radiation’s Affect on Salivary Glands
Which salivary gland is more susceptible to stone formation and why?
Salivary stones occur most commonly in the submandibular glands (80%–90%), followed by the parotid (5%–15%) and sublingual (2%–5%) glands, and only very rarely occur in the minor salivary glands.
The higher rate of stone formation in the submandibular gland is due to a few reasons [3]:
- The submandibular duct (Wharton’s duct) is longer than other salivary ducts. That means that saliva secretions travel further before being discharged into the mouth.
- The Wharton’s duct possesses two curves, at the posterior border of the mylohyoid muscle and near the duct orifice. The flow of saliva from the submandibular gland is often against gravity due to the location of the duct orifice is higher than the gland.
- The submandibular gland orifice itself is smaller than that of the parotid.
Related Reading: Diagnosing Xerostomia and Salivary Gland Hypofunction (SGH)
What are the salivary stones symptoms?
In general, the degree of symptoms depends on the extent of salivary duct obstruction and if there is a secondary infection. Patients with salivary stones most commonly present with:
1. Swelling
Salivary gland swelling upon eating. This swelling happens because the stone entirely or partially blocks the flow of saliva.
The gland’s swelling will subside when salivary stimulation ceases, and saliva is secreted out of the gland. Depend on the stone’s size, and this may take a few minutes to a few hours.
As described in the formation of the stone section above, stasis of the saliva may lead to the inflowing of bacteria into the gland causing infection, fibrosis, and gland atrophy.
2. Pain
Since the glands are encapsulated, and there is little space for expansion, the saliva’s retention will cause pain unless the stone is small and does not significantly saliva retention.
3. Infection
There may be expressible suppurative or non-suppurative drainage and erythema or warmth in the overlying skin if there is an infection.
Like what you’re learning? Download a brochure for our online, postgraduate Orofacial Pain and Oral Medicine degree program.
Clinical Steps to Diagnose Salivary Stones
1. Bimanual Palpation
The first step is bimanual palpation directed in a posterior to anterior fashion along the course of the involved duct, and it may be possible to detect a stone.
2. Plain Film Radiographs
Plain film radiographs are helpful to visualize stones. But the question is they are inexpensive, readily available, and result in minimal radiation exposure.
Can salivary stone detect on plain radiography?
It is essential to understand that 50% of parotid gland stones and 20% of submandibular gland stones are poorly calcified [4]. This is clinically significant as these poorly calcified stones will not be detected radiographically.
3. Conventional Sialography
A catheter will be inserted through the duct opening oil, or water-based iodine contrast will be instilled. Then imaging using panoramic, CBCT, CT images, or MRI will be used. Sialolith will look like a void in the sialography image.
4. Ultrasound
Ultrasound is widely used as a first-line imaging modality to assess the presence of salivary gland stone. It is safe as no radiation is involved in the modality, less costly than other imaging, and can visualize large stones.
5. CT Scan
CT images have higher sensitivity than plain film radiography for detecting salivary stones using a slice thickness of 0.2– 0.5 mm.
6. CBCT Scan
CBCT can be used, and it has the advantages of reduced superimpositions and distortions of the panoramic image and reduced radiation exposure over medical CT.
7. Sialendoscopy
Sialendoscopy can be used as a diagnostic and therapeutic technique for salivary gland stones. Its advantages include allowing visualization of the duct canal and segments of a duct and removing stone if possible.
How are salivary stones treated?
Treatment starts with managing the acute phase using analgesics, hydration, and antipyretics, as necessary. If the stone is noticed near the duct’s orifice and it has a small size, sialogogues such as sugarless lemon troches, massage, and heat applied to the affected area may also be beneficial to eject the stone outside.
Big stones or the stones located in the posterior portion of the duct can be removed by surgery. Small stones can be removed by sialendoscopy. In the case of intraparenchymal stones, sialoadenectomy remains a treatment option. Sialoadenectomy remains the last treatment option in case of failure of refractory intraparenchymal stones.
Step-by-Step Procedure for Removing a Sialolith from the Submandibular Gland

Figure 2. Image courtesy of Dr. Al-Eryani, Orofacial Pain and Oral Medicine Center, Herman Ostrow School of Dentistry of USC
This procedure is done when the stone is in the anterior part of the submandibular duct:
1. Identify the Location of the Stone
Gentle palpation should be done to get a sense of the location and border of the stone. If the stone is touchable and visible in the submandibular duct’s anterior part, surgical removal of the stone is possible under local anesthesia. Otherwise, the patient should be referred, and no surgery should be performed. (Fig. 1)
2. Prepare Your Instruments
The basic instruments you need for stone removal include:
- Local anesthetic cartridge and syringe
- Scalpel: Blade handle with the disposable blade or a disposable scalpel
- In the mouth, the #15 and #12 blades are most commonly used
- Tissue forceps without teeth
- Retractor
- Needle holder and suture: 4-0 silk sutures are commonly used
- Scissors
- Gauze
- Curved forceps and bite block (as needed)
- Specimen bottle with fixing solution and biopsy datasheet (if tissue other than stone is collected)
3. Administer Anesthesia
In general, patients are afraid and nervous about any surgical procedures. The more pain control you achieve, the more likely the procedure will be successful. Use both topical and local anesthesia infiltration in an attempt to obtain less or no pain to the patient during the procedure.
Note: Do not rush to the next step. Take enough time for the local anesthesia to work.
4. Excise the Stone
After localization of the stone, a traction suture is placed underneath the duct and posterior to the sialolith.
Then, after the suture is retracted upwards, an incision is made at the duct along its long axis, resulting in spontaneous exposure of the sialolith. The incision must avoid the duct orifice.
Next, use the tissue forceps to remove the stone. Most of the time, no suture for the wound will be needed. Then, examine the removed sialolith and if a tissue is collected, send it to the oral pathology lab. (Fig.2).
Earn a Master’s Degree in Orofacial Pain and Oral Medicine Online
Like what you’re learning? Consider enrolling in the Herman Ostrow School of Dentistry of USC’s online, competency-based 1-year certificate program or 3-year Master’s program in Orofacial Pain and Oral Medicine.
References
1. Huoh, K.C. and D.W. Eisele, Etiologic factors in sialolithiasis. Otolaryngol Head Neck Surg, 2011. 145(6): p. 935-9.
2. Liu, B., et al., Xerostomia and salivary hypofunction in vulnerable elders: prevalence and etiology. Oral Surg Oral Med Oral Pathol Oral Radiol, 2012. 114(1): p. 52-60.
3. St. Louis, M., Contemporary Oral, and Maxillofacial Surgery. Mosby Elsevier. pp. 398, 407–409, 2008.
4. Haring, J.I., Diagnosing salivary stones. J Am Dent Assoc, 1991. 122(5): p. 75-6.

