Erythema multiforme (EM): First described in 1866 by Ferdinand von Hebra as an acute, self-limited cutaneous disease characterized by multiform skin lesions, now called EM minor [1]. In 1950, Bernard A. Thomas classified EM into erythema multiforme minor (von Hebra)...
Kamal Al-Eryani, DDS, PhD
How to Diagnose and Remove Salivary Stones (Sialoliths)
What are salivary stones? Salivary stones, also called sialoliths, are calcified organic masses that form within the salivary gland's secretory system. Salivary stones comprise of organic and inorganic materials, including calcium carbonates and phosphates, cellular...
Oral Laser Ablation Surgery: Step-by-Step Guide for Dentists
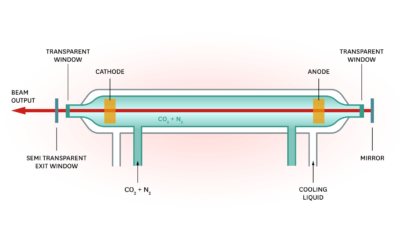
What is a laser? Lasers are an intense, high energy, coherent (travels in a constant phase in time and space), monochromatic (a single wavelength particular to the medium), and collimated (travels in the same direction) electromagnetic radiation that is produced by a...
Step-by-Step Instructions for Performing Oral Cryotherapy
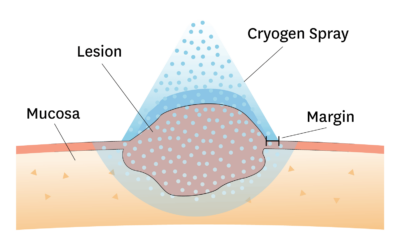
Oral Cryotherapy Oral cryotherapy is a very safe, easy to perform, and relatively inexpensive treatment for various selected oral lesions. You should never perform cryotherapy unless you know the diagnosis of the lesion you to freeze. HPV is associated with papillary...
Minor Salivary Gland Biopsy for Diagnosing Sjogren’s Syndrome
Minor Salivary Gland (MSG) Biopsy Minor salivary gland (MSG) biopsy of the lower lip mucosa is used to confirm the diagnosis of Sjogren’s syndrome. Sjogren’s is a chronic autoimmune disorder involving the destruction of glandular tissue. Sjögren's syndrome can cause...
How to Conduct an Oral Cavity Punch Biopsy
What is a punch biopsy? An oral cavity punch biopsy is considered the primary technique to obtain diagnostic, full thickness skin specimens. It is performed using a circular blade or trephine attached to a pencil-like handle. The instrument is rotated down through...
How to Perform an Oral Biopsy
A biopsy is defined as the sampling or removal of tissues or liquids from the body for examination, in order to determine the existence or cause of a disease. A biopsy is strongly recommended for most of the lesions that persist for more than two weeks which...