Facial sweat is a natural bodily response that helps regulate body temperature and maintain overall health. However, excessive facial sweating can be a source of concern for many individuals, leading to discomfort, embarrassment, and self-consciousness. Some causes of...
Mariela Padilla
Exploring Carotidynia: Symptoms, Diagnosis, and Treatment Options
In 1927, Fay described a painful condition over the common carotid bifurcation, without any structural abnormality. The condition was described as Fay’s Syndrome or Idiopathic Carotidynia. The pain is located in the anterior part of the neck, over the bifurcation of...
Circadian Rhythms: When the Pain Comes at the Same Time
Circadian rhythms are physical, mental, and behavioral changes that follow a 24-hour cycle. These natural processes respond primarily to light and dark and affect most living things, including animals, plants, and microbes. Biological clocks are organisms’ natural...
Understanding the Role of Alpha Receptors in Pain Management
α1-adrenergic alpha receptors are G-Protein Coupled Receptors that are involved in neurotransmission and regulate the sympathetic nervous system through binding and activating the neurotransmitter, norepinephrine, and the neurohormone, epinephrine. This receptor plays...
Indomethacin Responsive Headaches
The indomethacin-responsive headache disorders consist of a group of conditions with a particularly good response to indomethacin. Two of the trigeminal autonomic cephalalgias are included, which are hemicrania continua and paroxysmal hemicrania. Other conditions are...
Can You Get a Headache From Headache Medication?
People with a primary headache disorder, such as migraine or tension-type headache, might be experiencing undesirable pain secondary to the intake of acute headache medication. This is called a medication overuse headache (MOH) or transformed headache. MOH is a...
The Blinking Eye
Blepharospasm [aka, blinking eye] is a focal dystonia involving the orbicularis muscle causing repeated and abnormal movements of the eyelids. Patients with blepharospasm may be characterized by various types of involuntary activation of periocular muscles, and not...
A Glimpse into Occipital Neuralgia
If the patient experiences a sharp pain in the back of the neck, close to the nuchal line, and it radiates to the parietal and frontal areas, the clinician should consider the possibility of occipital neuralgia. Occipital neuralgia (ON) is a primary headache disorder...
CGRP: 4 Letters That Became a New Frontier in Pain Management
What Does CGRP Stand For? Calcitonin gene-related peptide (CGRP) is a neuropeptide (neurotransmitter of the nervous system) discovered over 30 years ago. It has specific receptors located both centrally and in the periphery. CGRP is present in trigeminal neurons and...
3 Elements of General Neck Examination
The evaluation of the neck provides useful information for the dental practitioner by identifying conditions that might contribute to the oral health of the patient and the appropriate function of the masticatory system. At the same time, it constitutes a triage,...
How to Insert and Adjust Occlusal Stabilization Appliances
There are four primary elements that form the theoretical basis for an occlusal stabilization appliance: It protects teeth from wear It stabilizes an unstable bite It makes the patient more aware of any oral habit It allows you to reduce loading on a specific...
How to Perform a TMJ Injection
TMJ injections are performed with corticosteroid and anesthetic to produce a two-fold effect: one reduce inflammation with the corticosteroid (triamcinolone acetonide) and two produce anesthesia or pain relief using lidocaine 2% without epinephrine. Corticosteriod is...
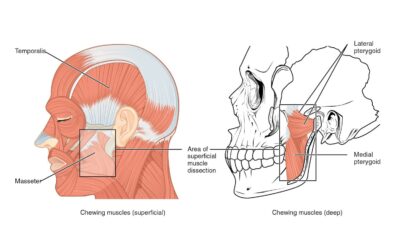
How to Measure Orofacial Pain With a Muscle Tenderness Exam
In this article, we review ways to assess muscle tenderness and pain. Common abnormalities of the masticatory muscle include injection induced myositis, myofascial taut band, trigger point, hypertrophy, spasms, etc. Note: Prior to each procedure, introduce yourself...
How to Conduct a Cranial Nerve Examination
The following equipment is required for a Cranial Nerve Examination: Cotton ball Safety pin Pen torch (source of light) Tongue blade Tuning fork (512 Hz) 1.) Olfactory Nerve (I) The olfactory is a sensory nerve, and damage in the nasal epithelium or the basal...
Closed Lock Mobilization: TMJ Exercises & Stretches
In this article, we'll provice step-by-step TMJ exercises and treatments for Dentists and self-mobilization stretches for patients. The main reason why a jaw locks closed is due to a derangement of the TM joint (disk displacement without reduction or DDNR). It is...
How to Perform an Occlusal Analysis
Occlusion, simply defined, is how teeth meet when the lower and upper jaw come together. Proper occlusion is necessary for eating, aesthetics, and disease prevention. However, many factors can cause malocclusion including trauma and genetics. Before we cover the...
TMJ Assessment: Jaw Range of Motion, Noise, and Tenderness
For TMJ mobilization procedures read: Closed Lock Mobilization: TMJ Exercises & Stretches. Jaw Range of Motion Assessment Prior to the procedure, introduce yourself to the patient, explain the purpose of the examination, obtain consent, and be sure to meet...
How to Perform a Lymph Node Examination
Lymph Node Examination A lymph node evaluation should be included in all new patients as part of the oral cancer triage. Below is a video showing the proper technique and a written explanation of what is expected from dentists when performing a lymph node and...