Oral cancer is a significant public health problem worldwide, ranking as the 6th most common cancer with a 5-year survival rate of 50% [1]. It accounts for roughly 3% of all cancers diagnosed annually in the United States. On average, 90% of these cases are oral...
When to See a Dermatologist for Lichen Planus
Lichen planus (LP) is an immune-mediated disease with an unknown etiology. Its clinical presentation waxes and wanes, and its severity goes from symptomatic oral erosions with erythema to asymptomatic white striations. In the oral cavity, the locations of these...
Common Viruses of the mouth: Herpes Simplex Viruses 1 and 2
Common viruses that can be present in the oral cavity are Herpes Simplex 1 and 2. Herpes Simplex Virus Type 1 (HSV-1) is spread predominantly through infected saliva or active perioral lesions. HSV-1 is adapted best and performs more efficiently in the oral, facial,...
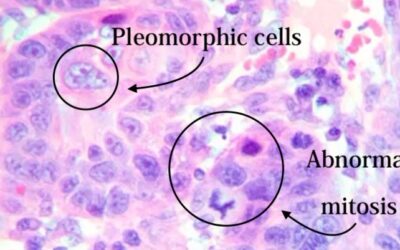
Squamous Cell Carcinoma: A Silent Killer
Squamous Cell Carcinoma is a deadly malignancy disease that primarily affects the oral cavity tissue and accounts for more than 90% of all oral malignancies [1]. OSCC dramatically affects patients’ quality of life, resulting in high morbidity and mortality rates. The...
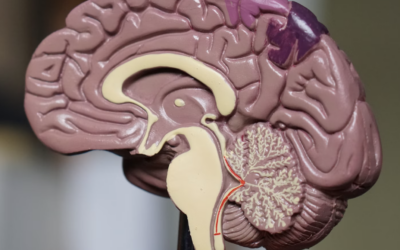
Exploring the World of Oral and Maxillofacial Pathology and Radiology
Oral and Maxillofacial Pathology is a specialized field in dentistry and pathology that focuses on understanding, identifying, and treating diseases that impact the oral and maxillofacial region. It involves investigating the reasons behind these diseases, how they...
A Closer Look at MRONJ: Medications, Risks, and Dental Management
Osteonecrosis of the jaw (ONJ) occurs when there is damage to the bone that interrupts the nutrient supply or because of a medical condition that reduces bone health (Sedghizadeh, 2009). When the ONJ is associated with medications, it will be referred to as...
HPV Uncovered: Vaccination, Oral Lesions, and Comprehensive Care
Human Papillomavirus (HPV) is an infectious disease that can cause lesions in the genital and oropharyngeal areas. It is considered the most common sexually transmitted infection (STI) in the United States. Besides being spread horizontally between individuals,...
White Oral Lesions That Need Your Attention
White lesions, also known as "white patches," in the oral cavity refer to abnormal areas of the oral mucosa that have a white or whitish appearance. They may present as patches or plaques on the soft tissues inside the mouth. White lesions can arise from various...
Why is a Tongue Evaluation Important?
Your mouth is one of your body’s most important warning systems. Tongue lesions may indicate a local disease process or an overall systemic issue. Approximately 15.5 percent of US adults present with tongue lesions according to the National Health and Nutrition...
Neurological Consequences of COVID-19
The knowledge and understanding of COVID-19 and its consequences is progressing, giving better insight into the heterogeneous nature of its acute and long-term effects. The available evidence on the pulmonary, cardiovascular, neurological, hematological, multisystem...
Clinical Features, Diagnosis, and Treatment of Erythema Multiforme
Erythema multiforme (EM): First described in 1866 by Ferdinand von Hebra as an acute, self-limited cutaneous disease characterized by multiform skin lesions, now called EM minor [1]. In 1950, Bernard A. Thomas classified EM into erythema multiforme minor (von Hebra)...
How to Perform an Oral Cyst Aspiration and Cytologic Smear
Cyst Aspiration A cyst is a membranous sac or cavity of abnormal character containing fluid. Indications for an Oral Cyst Aspiration For a jaw bone cyst lesion or any large soft tissue oral mucogingival cyst, aspirate the cyst aspiration. To help diagnosis of...
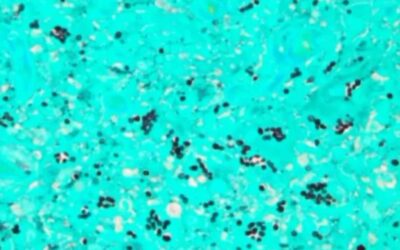
How to Perform an Agar Slant Culture Test for Fungal Infections
The Sabouraud Agar Slant Culture test is used when fungal overgrowth of the oral tissues is suspected, and is used to confirm the diagnosis of a fungal infection. Other adjunctive methods for the diagnosis of oral candidiasis include exfoliative cytology using...
A Dentist’s Guide: Oral Pathology of Vesicular Ulcerative Conditions
Explore a variety of vesicular ulcerative conditions of the oral cavity including common conditions such as Herpes, Syphilis, Aphthous Stomatitis, and Squamous Cell Carcinomas, and rare oral diseases such as Pemphigus Vulgaris, Mucous Membrane Pemphigoid,...
Oral Pathology of Primary, Secondary, and Tertiary Syphilis
Syphilis is actually on the rise, and there is a slight increase in the number of incidents of syphilis recently. California is the second most frequent location in the United States behind New York. Don't have time to read this article? We get it. Download the...
Infectious Lesions of the Oral Cavity: Histoplasmosis & Mucormycosis
So we talked about traumatic ulcerations we talked about squamous cell carcinoma, and OPSCC and HPV. Now we're going to talk about infectious ulcerative lesions including Histoplasmosis and Mucurmycosis. If you're looking for a clinical test to confirm a fungal...
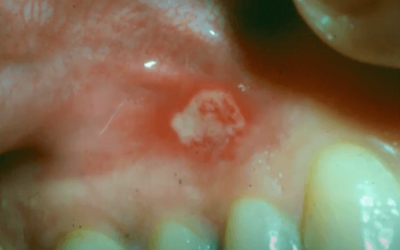
Squamous Cell Carcinoma Pictures of the Oral Cavity
In our previous two articles, Oral pathology of Oral Cavity and Oropharyngeal Squamous Cell Carcinoma, and Oral Pathology of Oral Pharyngeal Squamous Cell Carcinoma and HPV, we looked at histological images, discussed biological profiles, trends, survival rates, and...
Oral Pathology of Oral Pharyngeal Squamous Cell Carcinoma & HPV
OPSCC in HPV Positive vs. HPV Negative Patients You have oral cavity squamous cell carcinoma that is still related to smoking and drinking. Because there is less male smoking and more female smoking it is evening out the incidence of squamous cell carcinoma in the...
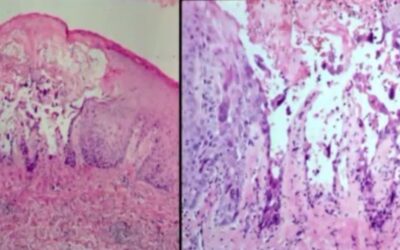
Oral Pathology of Oropharyngeal Squamous Cell Carcinoma
In contrast to Traumatic Ulcerative Granuloma with Stromal Eosinophilia, these lesions are squamous cell carcinomas of the tongue. They can look similar, but squamous cell carcinomas are a bit more involved. Don't have time to read this article? We get it. Download...
Oral Pathology of Traumatic Ulcerative Granuloma and TUGSE
In this article we'll review pictures from a patient that had a dental procedure and then a few days later noticed concerning ulcerations on their lip resulting from post-operative trauma. Don't have time to read this article? We get it. Download the Diagnosing...
Oral Pathology of Aphthous Stomatitis and Crohn’s Disease
Sometimes patients will present with recurrent ulcerations of the oral cavity, and the frequency and severity are alarming. When this occurs you have to start thinking of factors that might cause these alterations. Don't have time to read this article? We get it....
Aphthous Stomatitis: Treatment, Diagnosis, and Clinical Pictures
In this blog, we will teach you how to diagnose and treat Aphthous Stomatitis and its' three main subtypes: minor, major, and herpetiform aphthae. Don't have time to read this article? We get it. Download the Diagnosing Vesicular Ulcerative Conditions checklist to get...
Oral Pathology of Secondary (Recurrent) Herpetic Eruptions
This can be understood as the migration of virus from ganglion to surface along the course of sensory nerves. Upon reaching the surface the herpes virus infects epithelial cells and reproduces. Secondary or recurrent herpes is something that most of us are familiar...
Understanding Oral Herpes: Primary Herpetic Gingivostomatitis
There are many different types of herpes virus. Additionally, you have your Zoster Virus, Epstein-barr virus associated with mononucleosis, and some lymphomas. You've got Cytomegalovirus, again mono-like syndrome, Roseola which is associated with Heck's disease, and...