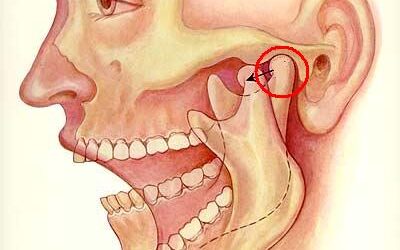
The temporomandibular joint (TMJ) comprises the mandibular condyle and the glenoid fossa of the temporal bone, covered by fibrocartilage, which provides greater resilience and support to mechanical stress [1]. This joint can be affected by bone deterioration, causing...
Compliance in Online Teaching: A Case Study of Orofacial Pain Program at Ostrow School of Dentistry
In recent years, and especially during the COVID-19 pandemic, the landscape of higher education has undergone a significant transformation with the proliferation of online learning platforms and the increasing demand for flexible educational opportunities. In response...
Diagnosing TMD: When to Consider a Rheumatological Referral
Painful temporomandibular disorder (TMD) stands as a prevalent source of orofacial pain, affecting 5-12% of US adults. As dentists, our encounters with TMD cases are frequent, with patients presenting discomfort, audible sounds, or limitations in jaw movement. Despite...
TMJ Clicking Causes, Symptoms, and Diagnosis
The temporomandibular joint (TMJ) is one of the most complex joints in the body. It is considered a ginglymoarthrodial joint because it provides rotation (ginglymoid) and translation (arthrodial) movements [1]. It is formed by the mandibular condyle and the temporal...
Salivary Gland Tumors: Rarity, Risks, and Treatment Insights
Salivary glands are exocrine glands that produce saliva in the oral cavity. The major salivary glands are parotid, submandibular, and sublingual. The minor salivary glands line the oral mucosa and the upper digestive tract. Salivary gland tumors are uncommon. The most...
Oral Medicine Specialists for Complex Health Conditions
Oral medicine was recently acknowledged as the 11th ADA-recognized specialty in dentistry. The American Academy of Oral Medicine defines oral medicine as the specialty of dentistry responsible for the oral health care of medically complex patients and for diagnosing...
Orofacial Pain Specialists and Solutions
Orofacial pain specialists are dentists who diagnose and treat orofacial pain disorders. Orofacial Pain (OFP) is the latest specialty of dentistry recognized by the National Commission on Recognition of Dental Specialties and Certifying Boards. In 2020, this...
Unmasking Excessive Facial Sweating
Facial sweat is a natural bodily response that helps regulate body temperature and maintain overall health. However, excessive facial sweating can be a source of concern for many individuals, leading to discomfort, embarrassment, and self-consciousness. Some causes of...
Exploring Carotidynia: Symptoms, Diagnosis, and Treatment Options
In 1927, Fay described a painful condition over the common carotid bifurcation, without any structural abnormality. The condition was described as Fay’s Syndrome or Idiopathic Carotidynia. The pain is located in the anterior part of the neck, over the bifurcation of...
Mandibular Advancement Devices for the Treatment of Obstructive Sleep Apnea
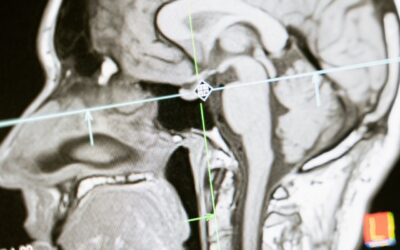
Obstructive Sleep Apnea (OSA) is a prevalent sleep disorder characterized by upper airway collapse during sleep. Continuous Positive Airway Pressure (CPAP) is the gold standard treatment, but its efficacy is hindered by low compliance. Oral appliances, specifically...
Unraveling Burning Mouth Syndrome: A Review of Diagnosis and Treatments
Burning mouth syndrome [BMS] is a chronic and challenging orofacial pain syndrome characterized by a persistent burning sensation in the oral mucosa, in the absence of specific oral lesions. It predominantly affects middle-aged and elderly women, often associated with...
Circadian Rhythms: When the Pain Comes at the Same Time
Circadian rhythms are physical, mental, and behavioral changes that follow a 24-hour cycle. These natural processes respond primarily to light and dark and affect most living things, including animals, plants, and microbes. Biological clocks are organisms’ natural...
Understanding the Role of Alpha Receptors in Pain Management
α1-adrenergic alpha receptors are G-Protein Coupled Receptors that are involved in neurotransmission and regulate the sympathetic nervous system through binding and activating the neurotransmitter, norepinephrine, and the neurohormone, epinephrine. This receptor plays...
Can Oral Lichen Planus (OLP) Look Like Oral Epithelial Dysplasia?
Oral lichen planus is an immune-mediated disease with unknown etiology. Its clinical presentation waxes and wanes, and its severity goes from symptomatic oral erosions with erythema to asymptomatic white striations. The locations of these clinical signs are more...
Indomethacin Responsive Headaches
The indomethacin-responsive headache disorders consist of a group of conditions with a particularly good response to indomethacin. Two of the trigeminal autonomic cephalalgias are included, which are hemicrania continua and paroxysmal hemicrania. Other conditions are...
What is Trigeminal Neuralgia and How is It Treated?
Trigeminal Neuralgia is an uncommon disorder characterized by recurrent attacks of lancinating pain in the trigeminal nerve distribution. Typically, brief attacks are triggered by talking, chewing, teeth brushing, shaving, a light touch, or even a cool...
What is Myofascial Pain Syndrome and How is It Treated?
Myofascial Pain (MPS) is a noninflammatory disorder of musculoskeletal origin, associated with pain and muscle stiffness, characterized by the presence of hyperirritable palpable nodules in the skeletal muscle fibers, which are termed MTrPs. These trigger points are...
How Do You Treat a Hypnic Headache?
Hypnic headaches also known as alarm clock headaches are a rare type of primary headache that occurs during sleep and tend to wake the person up, seen particularly in elders. These headaches only occur when a person is asleep (Sleep Foundation, 2023). Amongst patients...
Eagle’s Syndrome: What is It and How is It Treated?
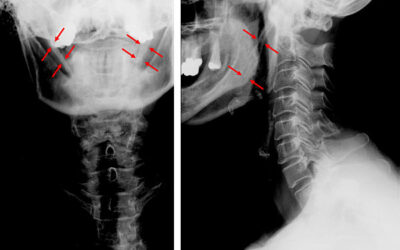
Eagle's syndrome, also known as stylohyoid syndrome, styloid syndrome, is caused by an elongated or disfigured styloid process, or a calcified stylohyoid ligament (Egierska D et al 2021). The abnormality or elongation leads to orofacial and cervical pain that are...
Can You Get a Headache From Headache Medication?
People with a primary headache disorder, such as migraine or tension-type headache, might be experiencing undesirable pain secondary to the intake of acute headache medication. This is called a medication overuse headache (MOH) or transformed headache. MOH is a...
Biofeedback Therapy for Chronic Pain
Biofeedback is a way for an individual to self-regulate their physiologic response to pain with the help of a feedback system. Patients can receive auditory, visual, or tactile feedback information about how their body is reacting (ie. muscle tension or heart rate)....
What Is Central Sensitization (CS)?
Central sensitization is an amplification of neural signaling within the central nervous system that elicits pain hypersensitivity. (Woolf, 2011). It is a pathological phenomenon that represents both structural and functional changes in the CNS and leads to increased...
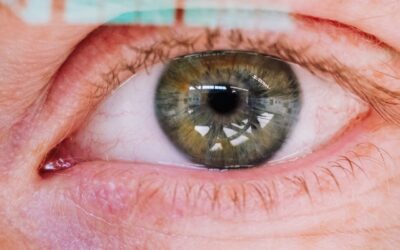
The Blinking Eye
Blepharospasm [aka, blinking eye] is a focal dystonia involving the orbicularis muscle causing repeated and abnormal movements of the eyelids. Patients with blepharospasm may be characterized by various types of involuntary activation of periocular muscles, and not...
Alpha-Lipoic Acid: Nature’s Relief for Burning Mouth Syndrome Sufferers
For those of you fortunate enough not to have heard of Burning Mouth Syndrome (BMS), let me introduce you to this debilitating pain condition. BMS is characterized by a burning sensation in the tongue and/or other oral mucosal areas. It is often associated with dry...