What is a jaw bone biopsy? When you use the term “bone biopsy,” this could mean you are taking a piece of bone or you are taking tissue that resides inside a bone. There are two approaches for a bone biopsy. A closed/needle bone biopsy involves inserting a needle...
Clinical Skills
How to Perform an Oral Cyst Aspiration and Cytologic Smear
Cyst Aspiration A cyst is a membranous sac or cavity of abnormal character containing fluid. Indications for an Oral Cyst Aspiration For a jaw bone cyst lesion or any large soft tissue oral mucogingival cyst, aspirate the cyst aspiration. To help diagnosis of...
Minor Salivary Gland Biopsy for Diagnosing Sjogren’s Syndrome
Minor Salivary Gland (MSG) Biopsy Minor salivary gland (MSG) biopsy of the lower lip mucosa is used to confirm the diagnosis of Sjogren’s syndrome. Sjogren’s is a chronic autoimmune disorder involving the destruction of glandular tissue. Sjögren's syndrome can cause...
How to Conduct an Oral Cavity Punch Biopsy
What is a punch biopsy? An oral cavity punch biopsy is considered the primary technique to obtain diagnostic, full thickness skin specimens. It is performed using a circular blade or trephine attached to a pencil-like handle. The instrument is rotated down through...
How to Perform an Oral Biopsy
A biopsy is defined as the sampling or removal of tissues or liquids from the body for examination, in order to determine the existence or cause of a disease. A biopsy is strongly recommended for most of the lesions that persist for more than two weeks which...
Trigger Point Mapping: Theory & Step-by-Step Technique
What is a trigger point? A trigger point is due to sensitized sensory nerves within a taut band of a muscle that when squeezed generates local and referred pain. The cause of a taut band is a hyperactive motor nerve branch, which generates sustained contraction in the...
How to Administer a Gingival Cold Test
This test is utilized when you have a focal, intraoral, probable neuropathic pain disorder involving a branch of the trigeminal nerve with palpable gingival allodynia/hyperalgesia and no obvious, local dental pathology exists such as tooth fractures, periapical...
How to Perform a TMJ Injection
TMJ injections are performed with corticosteroid and anesthetic to produce a two-fold effect: one reduce inflammation with the corticosteroid (triamcinolone acetonide) and two produce anesthesia or pain relief using lidocaine 2% without epinephrine. Corticosteriod is...
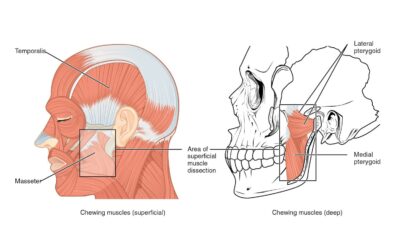
How to Measure Orofacial Pain With a Muscle Tenderness Exam
In this article, we review ways to assess muscle tenderness and pain. Common abnormalities of the masticatory muscle include injection induced myositis, myofascial taut band, trigger point, hypertrophy, spasms, etc. Note: Prior to each procedure, introduce yourself...
How to Perform an Agar Slant Culture Test for Fungal Infections
The Sabouraud Agar Slant Culture test is used when fungal overgrowth of the oral tissues is suspected, and is used to confirm the diagnosis of a fungal infection. Other adjunctive methods for the diagnosis of oral candidiasis include exfoliative cytology using...
How to Conduct a Cranial Nerve Examination
The following equipment is required for a Cranial Nerve Examination: Cotton ball Safety pin Pen torch (source of light) Tongue blade Tuning fork (512 Hz) 1.) Olfactory Nerve (I) The olfactory is a sensory nerve, and damage in the nasal epithelium or the basal...
Closed Lock Mobilization: TMJ Exercises & Stretches
In this article, we'll provice step-by-step TMJ exercises and treatments for Dentists and self-mobilization stretches for patients. The main reason why a jaw locks closed is due to a derangement of the TM joint (disk displacement without reduction or DDNR). It is...
How to Perform an Occlusal Analysis
Occlusion, simply defined, is how teeth meet when the lower and upper jaw come together. Proper occlusion is necessary for eating, aesthetics, and disease prevention. However, many factors can cause malocclusion including trauma and genetics. Before we cover the...
TMJ Assessment: Jaw Range of Motion, Noise, and Tenderness
For TMJ mobilization procedures read: Closed Lock Mobilization: TMJ Exercises & Stretches. Jaw Range of Motion Assessment Prior to the procedure, introduce yourself to the patient, explain the purpose of the examination, obtain consent, and be sure to meet...
How to Perform a Salivary Gland and Salivary Flow Exam
In previous articles, Dr. Roseann Mulligan explored Xerostomia, Salivary Gland Hypofunction, the role of saliva in older adults, and the causes of dry mouth including xerogenic medications and systemic diseases. In this article, we'll cover a few practical methods to...
How to Perform a Lymph Node Examination
Lymph Node Examination A lymph node evaluation should be included in all new patients as part of the oral cancer triage. Below is a video showing the proper technique and a written explanation of what is expected from dentists when performing a lymph node and...